Background: Cytoreduction utilizing hydroxyurea to achieve a hematocrit (HCT) <45% has improved clinical outcomes for patients with Polycythemia Vera (PV). Pharmacists, through a collaborative practice agreement with hematologists, are uniquely posited to act as physician extenders and therapeutically dose adjust hydroxyurea (HU). Since 2013, HU therapeutic drug monitoring for PV patients has been transitioned to pharmacists in our oral chemotherapy clinic. We conducted a retrospective cohort cross-over study to evaluate pharmacist versus physician HU management to achieve a therapeutic HCT <45%.
Methods: We retrospectively queried our institutional electronic medical record to identify patients diagnosed with PV with a documented ambulatory HU prescription. Additionally, patients' HU must have been managed by a physician (Phys) and subsequently crossed over to a pharmacist (PharmD) with at least two documented encounters by each clinician type. Hematological parameters for therapeutic drug monitoring are outlined in Table 1. Descriptive statistics were used for demographic information and a random effects model was used to evaluate HU management between Phys and PharmD. We fit a generalized linear regression model with random intercepts for each patient, using SAS's PROC GLIMMIX and Laplace approximation method t-test for a significant difference in probability of a therapeutic measurement between PharmD and Phys managed patients. Odd ratios were also calculated and adjusted for age and sex. Statistical analysis was performed using SAS (SAS9.4 SAS Institute, Cary, NC) and R software (The R Group, Vienna, Austria), with p<0.05 considered statistically significant.
Results: Between 1/1/2003 and 1/20/2020, 104 patients meet the inclusion criteria. This cohort was primarily female (53%), white (97%), and aged 71 years during PharmD management vs 69 years during Phys management. The median time of a patient's HU management by PharmD was 2.4 years (IQR 1.2-3.8), Phys was 0.7 years (IQR 0.02-4.2), and overall was 3.6 years (IQR 2-6.6). 3154 complete blood count measurements were collected in the PharmD cohort and 2007 were collected in the Phys cohort.
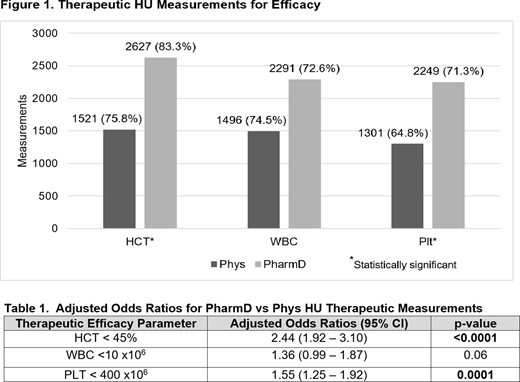
HU management by PharmD vs Phys resulted in statistically significant increases of therapeutic HCT measurements (p<0.0001) and platelet (PLT) measurements (p<0.0001) as shown in Figure 1. These outcomes remained significant when adjusted for both age and sex: HCT 87.8% vs 74.7% (p<0.0001) and PLT 78.4% vs 70.1% (p=0.0001). There was no difference white blood cell (WBC) therapeutic measurements between cohorts nor when adjusted for age and sex. Patients in the PharmD cohort had higher odds of achieving therapeutic HCT (OR 2.44; 95% CI [1.92 - 3.10], p<0.0001) and PLT (OR 1.55; 95% CI [1.25 - 1.92], p=0.0001) goals (Table 1).
In terms of hematological safety parameters, there was no significant difference in neutropenia (OR 1.30; CI 95% [0.51-3.25]) with PharmD vs Phys HU management. All grade neutropenia occurred in 35 (1.1%) and 18 (0.9%) of patients between the PharmD vs Phys cohort, respectively. Grade 3 neutropenia occurred in 1.1% of patients in both cohorts with no instances of Grade 4 neutropenia.
Conclusion: These findings support the efficacy of pharmacist therapeutic drug management of HU for patients with PV. Pharmacists managing HU achieve a target HCT and PLT count more often than physician management. By acting as a physician extender, pharmacist HU management for PV patients can help decrease the clinical burdens on physicians without compromising efficacy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal